Ministry of Health and Family Welfare
Always monitor and control blood sugar level: Advice for Diabetes Patients
Steroids a strict no-no for Mild COVID-19 patients: Director, AIIMS
Be Vigilant, Don’t Miss even Minor Symptoms, Stay Safe from Mucormycosis
Mumbai, May 21, 2021
Mucormycosis, also known as black fungus infection, is not a new disease. Such infections were reported even before the pandemic. Its incidence however was very low. Now, due to COVID-19, this rare but fatal fungal infection is being reported in large numbers. Coronavirus Disease Associated Mucormycosis (CAM) is being seen in patients who are either recovering or have recovered from COVID-19. Let us build on our earlier post on the topic , to learn what we can do to protect ourselves and our dear and near ones.
Director AIIMS, Dr. Randeep Guleria explained the increased incidence during a press conference last week. “Earlier, mucormycosis was commonly spotted in people suffering from diabetes mellitus, a condition where one’s blood sugar (glucose) levels are abnormally high. Cancer patients undergoing chemotherapy, those who have had a transplant, and people taking immunosuppressants (medications that weaken the immune system) also used to get it. But now due to COVID-19 and its treatment, an increase in number of cases is being witnessed. There are more than 20 cases of the fungal infection in AIIMS itself, all of whom are COVID positive. Many states have reported 400 to 500 cases, all among COVID patients.”
Why and how it affects COVID-19 patients during or post recovery?
Medicines used in treating COVID-19 tend to bring down the count of lymphocytes. Lymphocytes are one of the three types of white blood cells whose job is to defend our body against disease-causing pathogens such as bacteria, viruses, and parasites.The reduced count of lymphocytes leads to a medical condition called lymphopenia, making way for opportunistic fungal infection in COVID-19 patients.
There is a higher chance of occurrence of mucormycosis in patients whose immune system is not functioning well, and since COVID-19 treatment tends to suppress the working of the immune system, it places such patients at a higher risk of contracting the black fungus infection.
Disease and Symptoms:
Mucormycosis can be categorized depending on which organ of the human body it attacks. Signs and symptoms of the infection also vary depending on the affected body part.
- Rhino orbital cerebral Mucormycosis: Infection occurs when fungal spores are inhaled. It infects the nose, orbit of eye / eye socket, oral cavity and can even spread to the brain. Symptoms include headache, nasal congestion, nasal discharge (green colour), pain in sinus, bleeding nose, swelling on face, lack of sensation on face and skin discoloration.
- Pulmonary Mucormycosis: When spores are breathed in and reach the respiratory system, it affects the lungs. Symptoms are fever, chest pain, cough and coughing of blood.
The fungus can also infect gastrointestinal tract, skin, and other organs but the most common form is Rhino cerebral Mucormycosis.
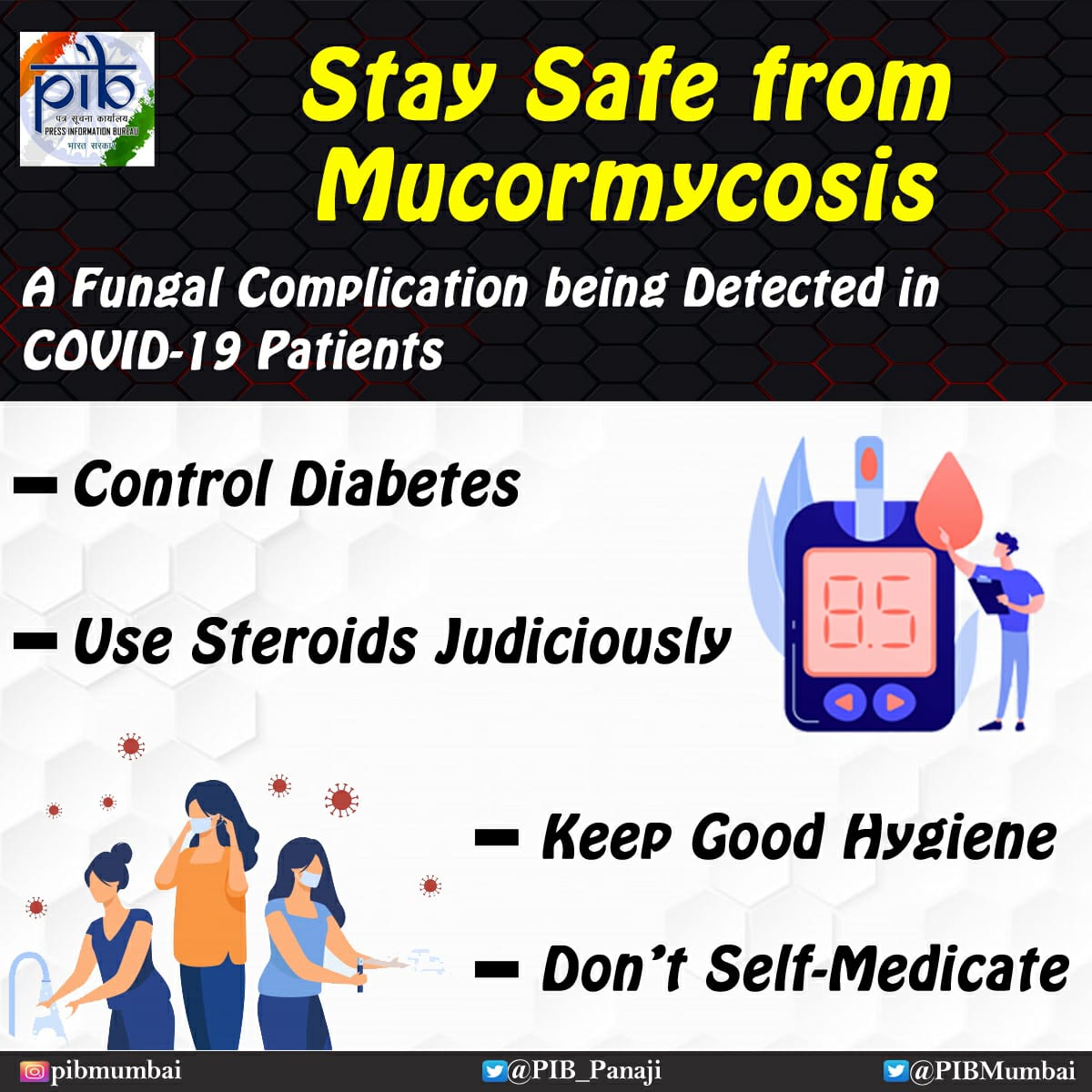
Preventive measures to be taken by COVID-19 patients:
People with following medical conditions should be more careful, they should constantly monitor their health and also take the following preventive measures.
Diabetic Patient (uncontrolled diabetes) + Steroid usage + COVID Positive – all three combined together places one under high risk of getting this infection. Hence diabetic patients should always monitor and control their blood sugar level.
Misuse of steroids is also a cause of concern that directly affects one’s immune system.
COVID Positive patients with mild form of the infection should strictly avoid taking steroids. On the one hand, steroids are of no use in treatment of mild COVID cases. On the other hand, taking steroids increases the risk of secondary infections like Mucormycosis. It leads to a high risk of fungal infection even after recovery from COVID-19. Hence if a COVID-infected person’s oxygen saturation level is normal, and he/she is categorized as clinically mild, steroids should be completely avoided.
Those who are taking steroids should also keep checking their blood sugar levels. In most cases, one who is not diabetic finds that after taking steroids, the blood sugar level shoots up to 300 to 400. Hence, it is essential to continuously monitor one’s sugar level.
“High dosage of steroids being taken by COVID-19 patients is of no use. Mild to moderate doses are good enough. As per the data, steroids should be given only for 5 to 10 days (maximum). Moreover, steroids increase the blood sugar level which can then become hard to control.” This can in turn increase the chance of fungal infection, said Prof. Guleria.
Wearing masks is compulsory. Fungal spores found in air can easily enter the body through the nose. This makes masking up doubly important, in preventing infection. People who work at or visit construction sites should specifically pay attention to this.
Where are these fungi found?
Mucormycosis is caused by a group of molds called mucormycetes. It is naturally found in air, water and even food. It enters the body through fungal spores from the air or can also occur on skin after a cut, burn, or skin injury.


An early detection of this infection can prevent potential loss of vision or brain infection in future.
Other Preventive measures to be followed:
|
Don’t miss even minor symptoms:
Pain and redness around eyes and nose, fever (usually mild), epistaxis (bleeding from the nose), nasal or sinus congestion, headache, cough, shortness of breath, vomiting of blood, altered mental status and partial loss of vision. |
Responsibilities of Doctors and other Health Care Workers
While discharging COVID-19 patients, advise about early symptoms or signs of Mucormycosis; such as facial pain, blockage, excessive discharge, loosening of teeth, chest pain and respiratory insufficiency. |

No comments:
Post a Comment